Waldenstrom's macroglobulinemia: Low Dose Rituxan
By Steve Kirsch
April 23, 2008
Update 5/10/15:
Rituxan comes in 10mL bottles with 100mg.
I am about 2 m2 per Body Surface Area Calculator.
So this suggests that 40mg would be an effective dose and could be administered once a week for 4 weeks ideally with something to eliminate bone marrow homing of WM and in conjunction with Ibrutinib to lower the IgM and reduce the flaring where the Ibrutinib is done prior to the Rituxan, but not at the same time (some in vitro studies show it may interfere with the killing).
Also, use CXCR4 inhibitor prior to the Rituxan if possible to get WM cells out of the marrow so they can be much more easily killed.
=====================
The proposal is for 20 mg/m2 done once a week.
Here is the argument.
Things we know:
- There is evidence that people who take the standard dose become resistant to future treatment.
- Being resistant to Rituxan should be avoided if at all possible because it is an effective drug at killing WM.
- There is evidence it kills cells expressing CD20 just as effectively as the 20X higher dose.
- The level of 20 mg/m2 supported by the ofatumumab concentration effectiveness curve (which shows no increase in impact above 10 ug/ml)
- It has worked in people who have tried it to reduce disease burden.
- There is ample data of significant shaving higher than this dosage. That should significantly and negatively impact the ability for Rituxan to be effective in subsequent doses since Rituxan must bind to the cell to enable it to be killed. If Rituxan can’t attach to cells, the cells can’t be killed.
- The Rituxan dosing was never picked for long term efficacy, but it was 100% based on whether people will tolerate it.
- There have not been any studies of whether lower dose Rituxan would be more or less effective than the standard dose.
- Giving people lots of Rituxan can cause a very significant IgM flare. This led to my losing vision in my left eye. Giving people no Rituxan causes no flare. One could logically conclude that the lower the Rituxan concentration, the lower the flare since, unless there is contrary evidence, most side effects in drugs are reduced by reducing the dosage. I can't think of any case ever where reducing the dosing of a drug produced greater side effects.
- A pilot study conducted by Dr. Ron Taylor and other researchers at the University of Virginia, during which CLL patients were given LDR by IV three times a week over four weeks, showed results ranging from stable disease to complete response (link at end of post, along with lots of other links). Not surprisingly, the complete responses were achieved in patients with the highest levels of CD20.
- One CLL patient has posted her experience online, pointing out that her absolute lymphocyte count (ALC) dropped from 137k to 4.6k after eight weeks of LDR at 30 mg, given intravenously three times a week. She had used standard-dose Rituxan in the past.
- Even at the drastically lower dosing, you can still get severe infusion reactions, so adequate premedication (usually Benadryl, Tagamet, Tylenol, and a steroid such as Solu-Cortef to reduce the inflammatory response) is a must although some people can do LDR with no premeds. Pre-treatment allopurinol and drinking lots of water, both of which help protect the kidneys from tumor lysis, which can happen when millions of cells die at once.
- You are protecting your kidneys more with LDR since you are lowering the number of dead cells it has to clear at any one time.
- 72 mg of methylprednisolone daily for a week may be synergistic to the the rituxan
- Phagocytosis becomes overwhelmed at levels above 30 mg and so b-cells escape death, get their rituxan eliminated by the liver, and return immune to further therapy.
- The massive killing at 375 dosing depletes complement. so these higher levels are very inefficient at killing cells. If you use such high levels, then you should infuse with 2 units of fresh plasma in order to increase complement available. Using lower-doses of Rituxan, so that complement does not become overwhelmed in the first place, is far more practical, as well as more cost effective.
- In our anecdotal CLL patient on LDR, he achieved better results with LDR than standard dose. Normally, retreating with Rituxan gives you less and less impact each time and that is exactly what happened. In his case he had plateaus of 2.3, 4.9, 5.1, etc. His most recent standard dose only got him to an ALC of 22.6 whereas LDR done after that allowed him to get down to 7.3 which is extraordinary.
- The initial intravenous infusion of one 20 mg dose of RTX promoted rapid clearance of more than 2/3 of circulating CLL cells from the peripheral blood in all patients (Figure 1A). This is 35X less than what is given for a standard Rituxan infusion.
- "Treatment of CLL patients with weekly RTX doses of 375 mg/m2 depletes complement (C) and induces substantial loss (~90%) of CD20 on circulating cells. This loss reduces the potential efficacy of RTX." Even as low as 60 mg/m2 gave 75% to 80% shaving.
- At a dose of only 20 mg/m2, you get less than 50% shaving which is much better than at 60 mg/m2, but shows just how much CD20 shaving you get with even low doses! This suggests that doses even lower are needed to minimize shaving!
- 20 mg/m2 does not deplete complement.
- ibrutinib strongly inhibited all cell-mediated mechanisms induced by anti-CD20 antibodies rituximab, ofatumumab or obinutuzumab
Therefore, all the data we know leads to the conclusion that it is more likely than not that the 375 dose is overkill and that lower doses should perform better due to the shaving effect.
Questions:
- Is there any evidence that contradicts any of the statements above?
- Do we have any reason to believe that by trying a lower dose that we’d be causing harm or creating worse outcome for the patient?
References:
Ibrutinib interferes with the cell-mediated anti-tumor activities of therapeutic CD20 antibodies: implications for combination therapy. So you want to use Ibrutinib to lower your IgM, then stop it prior to Rituxan.
Thrice-weekly low-dose rituximab decreases CD20 loss via shaving and promotes enhanced targeting in chronic lymphocytic leukemia is an interesting paper suggesting that 20 mg/m2 dosing (about 1/20th of the standard dose) promotes clearance without shaving. The first 30mg cleared 75% of cells in the bloodstream.
http://clldiary.blogspot.com/2007/04/low-dose-rituxan.html
http://clldiary.blogspot.com/2007/06/low-dose-rituxan-first-round-results.html: describes the switch to 2 days a week.His conclusion: "Well, folks, there’s a first time for everything. As far as I’m concerned, low-dose Rituxan is a no-brainer for most patients using the drug as a single agent. (I say this not only based upon my personal experience, but also upon Ron Taylor’s pilot studies and anecdotal reports from other patients.)"
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2817038/ discusses subcutaneous Rituxan injections.
http://abstracts.hematologylibrary.org/cgi/content/abstract/104/11/2520?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=1&author1=Taylor%2C+RP&andorexacttitle=and&andorexacttitleabs=and&andorexactfulltext=and&searchid=1&FIRSTINDEX=0&sortspec=relevance&resourcetype=HWCIT: treatment of CLL patients with weekly RTX doses of 375 mg/m2 depletes complement (C) and induces substantial loss (~90%) of CD20 on circulating cells which is not caused by B cell internalization or RTX masking of CD20 (Kennedy, J Immunol, 2004). This loss reduces the potential efficacy of RTX.Our results to date suggest that frequent but low dose RTX regimens can promote slow but steady cytotoxic attack of RTX on CD20 cells while preserving C activity and maintaining CD20 levels so that additional RTX treatments continue to be effective.
==========================
I was diagnosed with Waldenstrom's macroglobulinemia six months ago (see Waldenstrom's macroglobulinemia: Steve Kirsch's story).
I had 4 weekly doses of Rituxan which brought my serum IgM down to 2390 in just 3 months (it was 4290 before treatment)! I had an IgM flare that was treated with PP. See Kirsch Waldenstrom's Macroglobulinemia Diary. This happened on each round after the second infusion. Despite the recommendation of my doctor, I stopped my treatment after the second flare.
So what next?
I am working with Irene Ghobrial's lab at Dana Farber on collecting additional animal data to justify a different path that I think will be as effective, if not more so, with minimal side effects.
This page documents my reasoning for pursing a low-dose Rituxan regimen, rather than the standard dose.
This proposal has been read by Brian Druker (inventor of Gleevec) and Irene Ghobrial and Stephen Ansell (both prominent WM researchers) as well as others in the WM field. All of them thought it was logical and sounded quite reasonable to try. Even one of the most honored WM doctors, Robert Kyle, thought that the approach was "very reasonable." One doctor who has WM, Guy Sherwood, said he'd be willing to try it out on himself. In fact, everyone who has read it thinks it's worth a shot and would justify a clinical trial.
I just talked with Steve Treon at the IWMF Ed Forum who had great input all
of which I agree with.
First, he said if you try 1/2 the standard dose every 3 weeks, it might work
better or worse than what we have now, so it would definitely be an interesting
data point to see what happens.
He said we do know that keeping a high enough concentration in the blood for a
long time is key to getting a good result. A very low dose (e.g., 1/10) is
likely not going to have a good effect since the bone marrow concentration will
be too low.
It will not be possible to kill the WM cells while preserving the good B-cells
since the good B-cells are always easier to kill (because they are hit first
because they are in the blood) so you can't give a fractional dose expecting to
kill say 50% of the good B-cells and 50% of the WM cells; you'll always kill all
the good B-cells before you start killing the WM cells. That's an excellent
point and that hadn't occurred to me. So the "pea shooter" approach won't work;
there is way to save the good cells, so you might as well go for maximum
efficacy.
He said there is an unfortunate packaging issue with Rituxan combined with
medical laws means there is no cost savings here and the lab has to pour about
$10,000 of drug down the drain every time they do this. This is because they
package the Rituxan so you can give a reasonably heavy person 1 standard dose
with a little left over. You cannot use the excess drug on another patient. And
you must discard any unused drug within 24 hours. This means, you have to throw
half the bottle in the trash every time you do this just because Rituxan is
packaged and sold for the standard dose per patient. However, Rituxan is
packaged in 10mL and 50mL bottles, so if you want 300mg per dose (like I do),
it's just 3 of the small bottles with zero wasted drug!
He agreed that the amount of flare is likely proportional to the amount of
Rituxan so that reducing the dose should reduce the flare.
Finally, he also agreed I was a "challenging" patient. There appears to be
universal agreement on that one!
NOTE: I have not yet incorporated Treon's comments into the writeup below, so please keep this in mind.
I posted the link to this page to the IWMF Talklist and all of the comments so far have been very positive with the one exception of Tom Hoffman (people saying they want to try this on themselves too!). One reader told me due to travel problems, he was given Rituxan once every 2.5 weeks and he said it resulted in the lowest IgM level he's ever had and that he felt better after those treatments than he felt when they were given once a week. So there is precedence that deviating from the norm can give results that are as good as, if not better than, the standard protocol (which still has never optimized for efficacy!!!).
All drugs have side effects. Taking any drug is a tradeoff of efficacy vs. side effect. So, in my case, where the disease is life threatening, you want to choose a dose that maximizes efficacy, but not any more than that since there is no benefit and you risk side effects which, in general, increase as the dosage increases (although most docs claim that this isn't true for monoclonal antibody treatment).
The dosing of Rituxan for maximum efficacy is completely unknown. As David Maloney (from FHCC) explained to me, the current dosage was derived from the maximum tolerated dose under the assumption that "more must always be better." They found that 500mg/m2 was safe, so they wanted to give it in multiple doses, so the FDA told them it had to sum to less than 500mg/m2, so they divided by 4 to get 125mg/m2 and then they did dosing at 1X, 2X and 3X. They stopped at 3X and that's the standard dose: 375mg/m2. There was NO consideration of efficacy. In fact, no matter what your disease, no matter how aggressive or indolent it is growing, no matter what is affected, no matter what your age, and no matter how well you tolerate the drug or how fast your body clears it, . the prescription is almost exactly the same: 375mg/m2 once a week for 4 weeks. It's written in stone. Patient variation be damned. And if your body doesn't like it (e.g., you get an IgM flare), then they PP you in order to keep you on the schedule. So they manipulate the patient to match the non-optimized treatment protocol rather than modify the protocol to fit the individual patient.
So because the dosing was randomly chosen, it's almost a statistical certainty that the real optimum dose is different. My bet is the optimum dose is a lot less than they are giving you. But nobody knows the optimum dose for WM. I could be wrong and it could be more. It's only guaranteed that the current dose isn't optimized for me.
But we are never going to know if someone doesn't try out different dosings in order to calibrate the impact in my body.
And since 1) the chance I can be cured with the standard dosing is close to zero, and 2) it's super safe to take Rituxan at lower doses, I'm game for trying something different that might work better. No downsides other than a little lost time. But WM is slow moving. I've got time. So there is only upside (other than the risk of premature drug resistance)!
At the dosing they give you, the concentration in the blood is vastly more than what is needed to kill WM cells in the blood. People have verified this in vitro that doses much smaller than the standard dose have exactly the same effect. Irene Ghobrial at DFCI just verified it again recently.
One of the arguments I've heard for justifying the increased concentration is that you need the higher concentration in the bloodstream in order to get a high enough concentration in the bone marrow. Some doctors say if you set a blood stream concentration, the bone marrow concentration will equilibrate within a matter of hours. But others disagree. For example, consider Humira Pharmacokinetics which points out that the Humira concentration in synovial fluid range from 31% to 96% of those in serum. So if you take the more conservative view, the concentration in the bone marrow to equilibrate to the something less than the serum concentration after some reasonably short amount of time...maybe longer than a few hours, but probably within a couple of days. One thing is that this is very hard to measure the Rituxan concentration in the bone marrow. So there isn't a good way to definitively answer this important question. But we can get the answer through indirect observation of impact as described below.
As you'll see as you read on, there are many other unanswered questions. And there's the traditional medical profession Catch-22: you can't get a clinical trial approved if you don't have the data, and you can't get the data unless you do a clinical trial since animals are only a imprecise surrogate for humans.
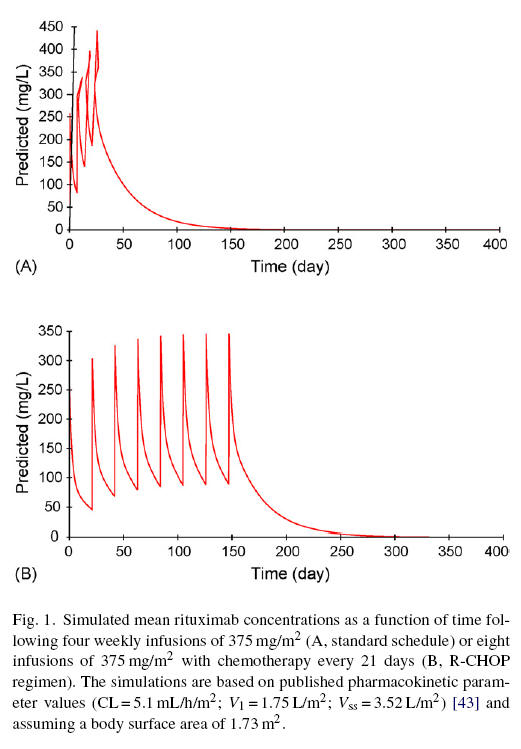
Naturally produced antibodies that are activated by an antigen have a blood
concentration of around 150μg/ml (see
ScienceDirect - Vaccine Safety and immunogenicity of a booster dose of
Staphylococcus aureus). Mononclonal CD-20 antibodies typically peak out in
max effectiveness at around 10μg/ml (see Fig. 1 in
Estimation of dose requirements for sustained in vivo activity of a
therapeutic human anti-CD20 antibody reproduced here which is for Humax, but the same
principles should apply to Rituxan). So beyond that concentration, you aren't
getting any benefit. However, the same paper points out that you need to start
with a higher concentration than this to deplete your B-cells because otherwise
your concentration is quickly depleted. So you start with a higher concentration
and once the existing CD20 cells are
depleted, then if you have a concentration of 10μg/ml at that point, you're
fine. Going much higher than 10μg/ml doesn't provide any benefit.
What's not known is the blood concentration to take the bone marrow to the
saturation concentration. This might be 3X higher if your concentration is
transient. If your concentration remains stable, the bone marrow should
equilibrate over time.
So beyond that concentration, you aren't
getting any benefit. However, the same paper points out that you need to start
with a higher concentration than this to deplete your B-cells because otherwise
your concentration is quickly depleted. So you start with a higher concentration
and once the existing CD20 cells are
depleted, then if you have a concentration of 10μg/ml at that point, you're
fine. Going much higher than 10μg/ml doesn't provide any benefit.
What's not known is the blood concentration to take the bone marrow to the
saturation concentration. This might be 3X higher if your concentration is
transient. If your concentration remains stable, the bone marrow should
equilibrate over time.
The concentration numbers seem reasonable compared to other monoclonal antibodies. For example, Humira Pharmacokinetics indicates a maximum serum concentration of 4.7μg/ml. So the numbers are pretty similar.
So to account for a reduction in concentration in the bone marrow, let's say you need to sustain and average of above 30μg/ml or so where the higher concentration is to get an effective concentration in the bone marrow. Well, you can do this with one infusion every 3 weeks at half the standard dose (see Fig. 1 of Pharmacokinetics of Rituxan reproduced below). Also, with that dosing schedule, the peak concentrations don't go much above 150μg/ml so your concentration always stays within at a safe, natural level for an antibody. I feel safer already!
What's even better is that once every 3 weeks is an approved dosage frequency since it's used with chemo, e.g., rCVP. And 8 continuous weeks of coverage with Rituxan is safe because its done now with chemo.
From the Cartron Pharmacokinetics of Rituxan paper, we have this graph where 1B is essentially what we'll have, just divide the Y axis numbers by 2 (it's not exactly 2 because the formulas used to calculate the graph are non-linear, but close enough). So your max concentration won't be any higher than naturally generated antibodies and your minimum concentration will stay above the 30μg/ml conservative minimum effectiveness level so you are always at effectiveness saturation, even if the bone marrow concentration is only 33% of the concentration in the circulating blood.
So the only thing experimental is using it without the chemo and halving the dose. Neither seem to be a big "stretch" especially considering that the dosing level for maximum efficacy has never been established for WM. Amazing isn't it? The drug was first approved by the FDA in 1997, almost 10 years ago and nobody's done any studies to find out if lowering the dose produces the same benefit. Considering each dose costs $25,000, you'd have thought someone would have checked into this by now.
But if we look hard enough, we find that in other diseases, halving the dose and tripling the time between infusions has already been proven both safe and extremely effective even when used for as long as 12 months! For example, in CLL, Consolidation and maintenance immunotherapy with r...[Cancer. 2008] shows you can give Rituxan just once a month at nearly 1/3 of the standard dose for a year and its both safe and remarkably effective.
Some argue that higher dosing for Rituxan can't hurt you and the higher dose ensures that you get at least the saturation concentration in your marrow. The argument is that side effects in Rituxan are all based on immunologic factors and are dose independent: you either react or you don't.
So other than potential safety, there are other benefits of low dosing: (1) cost/benefit and (2) potentially higher efficacy (you can wipe out more of the cancer), (3) minimizes the collateral damage on your immune system (the destruction of "good" CD20 B-cells), (4) a LOT less time sitting in the infusion chair (particularly important if you are like me and can't tolerate infusion rates higher than 125mg)
As far as cost goes, using the 1/2 dose every 3 weeks for a total of 8 infusions, you get 24 weeks of continuous coverage for the same cost as the 4 weeks. Of course, the tail drop off is longer in the "once a week case" but we're still looking at about 5 times or more extra coverage for the same cost to the insurance company. But you could argue that wasting the insurance company's money is a slam dunk since it's an approved protocol and spending their money far more efficiently and safely could result in a denial of coverage because it isn't an approved dosing level when administered once every 3 weeks. In short, insurance companies would rather overspend on something that is proven than save money on something that isn't.
As far as efficacy goes, there are at least three interesting examples where less is more.
- There is the Williams paper, Thrice-Weekly Low-Dose Rituximab Decreases CD20 Loss via Shaving and Promotes Enhanced Targeting in Chronic Lymphocytic Leukemia which shows that above the maximum effective dose, it's counter productive because you cause CD20 shaving in CLL. They found maximum efficacy is substantially lower than the MTD that everyone uses. It concludes low-dose Rituxan (administered 3 times a week to keep the concentration low and constant) is a more effective strategy in CLL than the standard dose.
- The Humira Pharmacokinetics article showed that that monoclonal antibody (Humira) was maximally effective at a dose of 40mg (about 5μg/ml) and that doubling the dose actually substantially reduced effectiveness! Also, 15% of patients took less than 1/10 of the standard 3mg/kg dose and it made no difference in outcome.
- Consolidation and maintenance immunotherapy with r...[Cancer. 2008] did even less than I'm suggesting in the maintenance phase and got great results. They did once a month at approximately a 60% reduction from the standard dose. So this is even more aggressive than I'm suggesting (lower dose, longer between doses, and it was for 12 months continuously instead of 24 weeks at a time) which proves that even 12 months of continuous coverage is safe.
The big argument for improved efficacy at lower dose is in the Williams paper. Some say that CD20 shaving would be more pronounced in CLL than WM because the CD20 is not as tightly bound as in WM. But nobody knows for sure if there is shaving or not in WM. The only way to find out is run the experiment at a lower dose. If shaving occurs in WM like in CLL, we could find that lowering the dose may substantially increase effectiveness. But we won't know until we try. And we can't try because we have the medical Catch-22 problem: no data means it is less likely that someone will approve the clinical trial (although clinical trial are sometimes approved on a good argument).
The other counter argument to the shaving is that the cell will regenerate the shaved protein within days, e.g., for normal cells it would be around 5 days. Nobody has a clue for how long a WM cell which has been shaved would take to regenerate the CD20. CD20 binding strength could be quite different in different strains of WM which might explain why some people show no response to Rituxan: if their CD20 is loosely bound and takes a long time to regenerate, hitting it with the huge "standard dose" of Rituxan strips all the CD20 and there is nothing left to target.
Also, if the Rituxan concentration is still too high when the protein regenerates, it might just get shaved off again. Only if your concentration is low enough when the protein regenerates would you have a chance to latch on to kill the cell.
Some docs don't buy the shaving argument at all, even in CLL. But even they admit that it could be true, but nobody knows and the medical Catch-22 ensures nobody will ever know unless there is some animal data to get people's attention to do the trial. We should have this soon.
The other argument for efficacy is time coverage. For most people, 4 weeks of coverage every 3 months is usually insufficient to get a deep remission. If there is a WM stem cell, we'll need pretty close to continuous coverage. If there isn't a WM stem cell, then we just need to kill the CD20 positive clone and we win. Obviously the current protocols don't do that consistently in patients so we really need to try something different and lower dosing for a long time seems like the most logical safest next thing to try in light of the data in other diseases.
The jury is out on whether there is a stem cell. One telling feature is how fast WM grows after the IgM has bottomed from Rituxan. If it grows at the original linear rate of x per month, there probably is a stem cell. If it grows at a rate proportional to IgM concentration, then if there is a WM stem cell, it's probably going to take a long time to regenerate the CD20 positive clone. I've heard clinicians say either can happen: linear rate or exponential rate. If that is true, then the only logical conclusion is that there probably is a stem cell but it's contribution to the disease may be significant or insignificant depending on the person. In either case, destroying all the the CD20 positive cells in the marrow is probably a good thing and if 4 weeks at a time isn't good enough, we need more time coverage.
I'm actually a good argument that if there is a stem cell, it is probably insignificant (see next section for details).
Another argument for lower dosing is Rituxan flare. I flare and it requires several rounds of PP which also has the effect of removing the Rituxan. So it's a no win. However, the flare is proportional to disease burden and I'm at half the level as before, so I should be reasonably safe even if I flare. Still, it's a bad thing.
Nobody knows whether the flare is proportional to Rituxan concentration. That's because they never vary the Rituxan concentration. So the lower peak concentration also has another wonderful potential benefit: reducing the amount and/or chance of an IgM flare caused by Rituxan.
Lastly, there are the unknown side effects that are related to Rituxan. The doctors claim that with a monoclonal antibody, all the known side effects are independent of concentration; you either react or you don't. I think the patients may have a different opinion. Patients report problems that coincided with Rituxan infusion and yet these are dismissed by clinicians as coincidence. This is always hard to know, but in general, my belief is less drug is safer and the only risk some have pointed out might be developing resistance but since there wasn't a problem with a low monthly dose for 12 months, I think this is a reasonable risk to take.
Measuring success
I dropped my WM by 50% in only 3 months with a single course of CPR and 3 extra infusions of Rituxan (once a week for 3 weeks; see my Diary). If my model of WM is correct (it's based on the cell line behavior), then it means I've killed a lot of LPC cells and thus the plasma cells never get "born." Since my WM plasma cells reduced by 50%, there are a number of different possibilities. If my WM plasma cell average lifetime is 6 months, then my treatment did a "perfect kill" of all the LPC cells in my marrow. If my WM plasma cell average lifetime is longer than that, then that's impossible since the max possible benefit in 3 months of a perfect treatment is a 50% IgM reduction. So I know only that my plasma cells live for 6 months or less.
This is actually really important because it means I can use my IgM level as a proxy for how effective the treatment is because the lifetime is reasonably short.
You can't do a PCR test for WM because it has to be specific to the WM cells and nobody has figured out what the specific marker is that defines a WM cell. And BMB's are way too expensive and inconvenient to do all the time.
It's also interesting because it answer the question I had for Treon of "how long do WM plasma cells live?" I now know the answer for me: 6 months or less.
The other good news for me is that this proves that any effect caused by a WM stem cell could be minor. We won't know for sure until my IgM drops more. But one thing is for certain from the data I now have: any WM stem cell contribution to my disease is certainly less than 50% (because if it was >50%, it would have been impossible to get a 50% reduction). And if WM plasma cells live for 6 months which is my guess based on the nadir of others, then the fact I got a 50% reduction in 3 months means that virtually all my WM is from the CD20 clone and if I kill that off, I'm in great shape. If my all my CD20 WM cells were generated from the stem cell, then a one month stoppage of the output of that generator would simply result in a 1/6 reduction in total IgM, not a 50% drop.
Also, I admit these numbers could be off. It's possible that the Rituxan just temporarily suppresses the rate of production of IgM by the WM plasma cells. But I think this is very unlikely since Rituxan causes IgM flare and when the Rituxan is removed, the cells go back to normal.
I also want to measure my Rituxan concentration right before the infusion after I've been doing it for 6 weeks or so to look at the bloodstream Rituxan concentration to verify it is where it should be. Each person is different. We probably do this once a year to make sure everything is working properly.
An even better variation of the treatment
A variation of the above that I think is really interesting is to do 1/10 the standard dose every 3 weeks. In fact, I think this may be a LOT better than what I've suggested above. How can that be?
Well, we shouldn't be obsessed with killing WM "instantly." I think that's a mistake. What's the rush?? This is a slow moving cancer. Why not kill it slowly, with minimal side effects and minimal impact on your immune system during treatment? I think can kill WM almost entirely in one year at a minimal Rituxan dose and it should work on most people even if they have bad reactions to the "standard" Rituxan dose or failed to respond to the normal dose. And you can keep taking the doses to keep the WM under control or stop for a while until the WM becomes detectable again.
So if I do 1/10 the standard dose every 3 weeks, right before each infusion, the bloodstream concentration is about 5μg/ml (it won't be quite that because things aren't exactly linear on Fig 1B, but it's a first approximation; someone smarter than me should run the numbers using the parameters in that paper). Because the concentration in the blood gets quite high and never gets below 5μg/ml, then I'd expect that the concentration in bone marrow is going to be higher than this because the average concentration outside the bone marrow is higher and the bone marrow will be slow to react to changes in the peripheral blood so it will have an averaging effect and reflect a time averaged concentration in the peripheral blood (doctors I've talked to vary on how insulated the bone marrow is from bloodstream concentration so if you have data on this, please let me know!).
With a lower dose, about 1/10 of the normal standard dose, I think the bone marrow concentration will then be in quite an optimal range for killing without risk of shaving. It may not be at 100% optimal, but that is actually what I want!!! Unlike what is being done today, I actually want my monthly kill % to be around 25%, not 100%! That's because the bone marrow makes good cells that are CD20 positive. I don't want to kill those good cells at all, but I'm willing to kill 25% of them a month. But with the standard treatment, the concentration is design to try to kill all of them. That's probably why they only have you on it for a month and then take a break. But that changes if we change the kill rate. All I do is reduce that volume by just 25% a month, not 100%. So instead of shutting off that small part of my immune system by complete elimination of new good CD20 like we do now, I just throttle it down by a measly 25%. So I minimally compromise my immunity during treatment which means I can treat continuously and with no risk of CD20 shaving. My IgM should thus drop every month little by little because at a 25%/month kill rate, the rate I'm killing the WM is far higher than the rate the WM is multiplying in the marrow. Since WM grows very slowly, a 25%/month kill rate will probably net out to be a 20% net reduction per month. My normal immune cells will only be reduced by 25% since they are generated from stem cells which aren't going to be killed by the Rituxan whereas the WM cells are generated from the dividing CD20 positive WM LPC clone.
But because WM is mostly created from the CD20 positive WM clone dividing in the bone marrow (and is not from a stem cell like every normal B-cell), the effect of just a 25%/mo kill rate of CD20+ cells on the WM clone is devastating. Assuming there is no WM stem cell or if there is one, a weak stem cell, (I've argued in the previous section that the stem cell component is probably immaterial, at least for me) and assuming most of the problem is from the CD20 positive WM cell dividing (which seems highly likely as I argued in the previous section), and that my WM is growing slower than 25% per month, then with low-dose Rituxan I have an optimized killing machine. I have next to no risk of shaving since the concentration is so low. People who might have been refractory to Rituxan from shaving because their CD20 is weakly bound for their WM) And if I'm killing just 25% of the WM cells per month, after 4 months, I'm down by 70%. After 8 months, I'm down by 90%. After 1 year I'm down by 97%! And I've minimized Rituxan flare, minimized side effects, minimized number of infusions (for a given amount of benefit received per infusion), minimized time spent to get the infusions, minimized cost to cure, maximized cure time, minimized the impact on your good immune system, and likely maximized the number of people who achieve a CR. Plus I've maximized people who can take the treatment because a lot of people can't take a lot of Rituxan. Infusion reactions also go away because the amount of drug is so small. So all the premeds can be either reduced or eliminated since the dose is so small (on subsequent doses. Your initial dose will need to be higher). The only risk I can think of with this approach is whether a low dose of Rituxan for 1 year can create drug resistance. But the Consolidation and maintenance immunotherapy with r...[Cancer. 2008] did 40% of the standard dose every month for a year without problem so I think this is pretty encouraging that we can avoid drug resistance.
Note: at 1/10 the standard dose every 3 weeks, my bone marrow concentration may still be too high (above 5μg/ml) so I may have to go lower on the Rituxan to achieve a concentration that will achieve the 25% kill rate that I want. But on the other hand, cells in the marrow are relatively protected from antibodies like Rituxan which seek to kill them so 1/10 may not be enough. We'll have to experiment with different levels. There is no way to predict this with the data we have today.
From a minimal collateral damage to normal cells perspective, the best dosing level will be about 1/2 the maximum WM kill rate. So we try adjusting the concentration upwards looking for a plateau in the kill rate. Then we use half that amount and verify that the kill rate is reduced by a 1/2 as well. This should thus cause minimal collateral damage to normal cells while continuously depleting the WM cells every month. However, reducing the dose from the maximum kill rate means the kill rate is slow and more time is required. The lower dose and longer time period puts you at higher risk for developing resistance to Rituxan (e.g., HAMA). So it's a tradeoff.
Summary of risks and benefits
Benefits of 1/2 to 1/10 dose every 3 or 4 weeks, i.e., using a pea shooter instead of an elephant gun to shoot down WM:
- I permanently lost vision in one eye because I flared (a high SV of 4.8 can cause permanent vision loss) and my physician didn't notice for almost a week. And I had the top WM specialist at Stanford! If it happened to me, it can happen to others. But the IgM flare is initiated only above a certain Rituxan concentration in the blood. A low dosing protocol might eliminate flare. Nobody can restore my sight, but maybe we can save the sight of others.
- Non-responders to Rituxan clear it much more quickly from the blood than responders. This could be cause or effect, nobody knows. But it could be that different people need drastically different concentrations of Rituxan to be effective. By not being afraid to try different levels, we can compare response rates within the same person. Wouldn't it be great if the standard protocol for Rituxan included a "dosing phase"? They do this with Bexxar, a similar drug. There's no reason we shouldn't do it with Rituxan.
- Rituxan monotherapy is, in general, effective in only 57% of NHL patients. If this change in the dosing can increase this percentage, the benefit is huge for everyone.
- Rituxan can cause serious side effects, some of them life-threatening. By using a much smaller dose, it's quite probable that we can reduce the incidence of this happening since a general medical principle is that reactions are proportional to dosage. Many argue this isn't true for mAbs; they claim you either react or you don't and it is independent of dose. I find that position hard to believe considering that with 4 doses, Grade 3 or 4 adverse effects were reported in 57% of patients and with 8 doses, 70% of patients reported Grade 3 or 4 adverse effects (see footnote 2 in PGxPredict™:RITUXIMAB).
- It would end the debate as to whether maintenance Rituxan is a placebo or effective. Today, there are some docs who refuse to prescribe maintenance R saying there is no evidence it is effective.
- It might change whether Rituxan should be given after CHOP. Right now, there are doctors who won't allow this.
- It might change whether Rituxan is given to pregnant women with WM. Right now, some doctors avoid doing this. But if the dose were lower it might make a difference.
- A ten times the benefit for a given dollar cost; this could be critical if you do not have insurance coverage for Rituxan (e.g., outside of the US).
- I believe flaring is proportional to the Rituxan concentration so reducing the dosage should totally eliminate flaring and also the need for periodic IgM monitoring (to detect a flare) and any plasmapheresis to fix the flare which also then compromises the efficacy of the treatment since the Rituxan is removed along with the IgM.
- If the dose is truly fractional of max efficacy, then there is less chance of problems from your immune system being compromised, e.g., shingles, actinic keratosis, etc.
- If shaving does happen, then there should be much higher efficacy per dose with this approach. You'd have the potential to virtually wipe out the cancer since more cells would be susceptible
- Because there should be less collateral damage to your good CD20, you should be able stay on it longer so you can wipe out more of the cancer at lower risk than the high dose protocol which reduces your IgG and IgA counts.
- A LOT less time sitting in the infusion chair (particularly important if you are like me and can't tolerate infusion rates higher than 125mg)
- Possible elimination of all hospital pre-meds (I bet due to the low dosage that you can just premed at home with Zantac and Claritin)
- Much better time coverage than the standard protocols; you are continuously kill WM cells rather than doing it in in discrete shots. If the most effective killing is done at low concentrations, this protocol should be way more effective on a per dose basis.
- Arguably higher safety since fewer drugs and lower concentrations
- Arguably fewer side effects, e.g., any post-infusion reactions should be negligible and reactions to the pre-meds would be reduced as well since less is required
- Visit the hospital less often (once every 3 weeks instead of once a week)
- Fewer undesirable side effects, e.g., hopefully, with the reduced dosage, your IgG and IgA shouldn't be impacted as much. This is important since low IgG, for example, can leave you very susceptible to bacterial pneumonias
- If Rituxan resistance is developed based on cumulative dose, then this is a huge breakthrough as it maximizes the impact you will have before you develop resistance.
- People seem to think that the standard protocol is a slam dunk, but it's possible that the standard protocol could be more likely to to resistance. For example, here's a posting from the IWMF talklist on May 12, 2008:
After 3, 1 x4 rituxan infusions over a period of 8 years, I was scheduled to start rituxan
maintenance, 4 every six months for two years. My counts are good and the onc felt this
was a good way(maintenance) to keep them there. After all the pre-meds
infusions(steroids, benadryl, allergy meds and the like) the rituxan infusions began.
Within 5 minutes, my face was hot and I had the worst chest pain immaginable. I felt
awful and then felt faint. My blood pressure, first high dropped to below 64 and I was in
real trouble. Needless to say the iv infusion of rituxan was stopped.
Risks
- Greater potential to develop immunity to Rituxan, e.g. HAMA But I don't think the link between low dosing and resistance has been established at all in the case of monoclonal antibodies like it is for other classes of drugs. However, about 60% of patients become resistant to the current Rituxan protocols anyway (see Monoclonal Antibodies for B-Cell Lymphomas: Rituximab and Beyond, Celeste Bello and Eduardo M. Sotomayor, Hematology (2007), pp 233-242).
- If it doesn't work, you've lost some time.
 If the dose is too high
and kills all your good B cells too, then you'll eliminate
all your good B-cells along with the WM and if you do that over a long
period of time, you could find yourself at a greater risk of diseases that
affect those with a compromised immune system. So lowering the dose and
giving it less frequently could actually be worse for you in this respect
than the standard dosing (which stops after two rounds). It only is a
benefit if the dose is sufficiently low to allow the good B-cells to live.
That's the key. However, fortunately, THAT can be easily measured via blood
tests (the so-called Rituxan panel) so you'd simply increasing the dosing of
the rituxan until you've reduced your normal B-cells, but NOT eliminated
them. That's the trick.
If the dose is too high
and kills all your good B cells too, then you'll eliminate
all your good B-cells along with the WM and if you do that over a long
period of time, you could find yourself at a greater risk of diseases that
affect those with a compromised immune system. So lowering the dose and
giving it less frequently could actually be worse for you in this respect
than the standard dosing (which stops after two rounds). It only is a
benefit if the dose is sufficiently low to allow the good B-cells to live.
That's the key. However, fortunately, THAT can be easily measured via blood
tests (the so-called Rituxan panel) so you'd simply increasing the dosing of
the rituxan until you've reduced your normal B-cells, but NOT eliminated
them. That's the trick.- It might work less well than the standard dosing. For example, the
figure on the right from
In vivo Targeting of
Human Neutralizing Antibodies against
CD55 and CD59 to Lymphoma Cells Increases the
Antitumor Activity of Rituximab was done in mice showing a single 150 μg dose in mice (the equivalent of the "standard dose" in humans) was way more effective than anything else. And what's really interesting is that two 25 doses (spaced 7 days apart) produced a significantly different impact than a single 50μg dose (first dose for each was given on the same day). Moreover, the shape of the 25+25 curve is very similar to the saline curve, but offset, suggesting it gives a more uniform benefit at any given point in time. It's also interesting that the single 50 dose gave a greater lifespan as compared with 25+25 which I didn't expect at all, but it could be explained by the cancer growing really fast so hitting it at the start was required to avoid death since in a week, a lot of mice die without treatment. So it's not really the same as WM which grows really slowly.
Bottom line
There could be 4 reasons that the current Rituxan treatment protocol fails to achieve a CR:
- CD20 shaving at high concentrations effectively neuters the treatment in some significant percentage of the cells
- The WM is very well protected in the marrow so you can only kill the easy stuff (which could explain why subsequent infusions are not as effective as you got the "low hanging fruit" at the start and subsequent infusions are going after the stuff that is more entrenched
- Stem cells could be constantly creating new WM clones so you are shooting at the wrong target
- Rituxan resistance develops where the WM cells in the marrow somehow figure out how to protect themselves (or you develop HAMA which eats the Rituxan right after it is injected)
The proposed method addresses #1 and #2 (due to more time covering the marrow with active antibody). Combining Rituxan with ADM3100 should also address #2. #4 could be made worse by this treatment.
I think it's worth trying Ritxuan once every 3 weeks at 1/10 the standard dose (per my "even better variation" section) for 8 infusions total and looking at the results. This results in 6 times the time coverage (24+ weeks instead of 4+ weeks), reduced peak concentration resulting in potentially fewer side effects including flaring, infusion related side effect, IgG and IgA lowering, and potentially higher efficacy due to reduced shaving and increased time coverage for a given amount of drug.
In short, if this doesn't work, the risk is that I've lost a little time and potentially developed resistance to Rituxan. It seems safe since higher and lower doses and rates and timeframes have been tried and are safe. And since it isn't clear that two 4X doses is clearly better than a single 4X dose, it looks like there is no downside since the alternative option (another 4 weekly doses) isn't clearly always better than doing nothing although the Response Duration does seem longer (See Table 2 in Extended rituximab therapy in Waldenström's macroglobulinemia). Also, I can always go back to trying the 4X weekly doses if this doesn't work.
The reason for doing it is to expand our knowledge and because of the potential for upside: a potentially more effective treatment (lower IgM and longer duration of response) due to the potential for reduced shaving, reduced chance of flare, and the longer time coverage for a given amount of drug. Also fewer needle sticks (which every patient loves).
One other really interesting benefit is that it's pretty much guaranteed that the concentration in the bone marrow will spend more time in the optimum concentration range (in the current protocol, the bone marrow concentration is probably always over the optimum level and there may be lots of CD20 shaving except at the very end when the infusions stop; but with this treatment, it's guaranteed that we will "pass through" the optimum concentration each and every time we do an infusion so you have 8 chances to win instead of 2).
So logically, it appears that it is a superior alternative to the standard 2nd 1x weekly x 4 treatment. We'll be monitoring progress and if it doesn't work, we can stop doing it. So the risk is extremely minimal.
Trying this out
First, wait until my IgM has stopped declining.
After two standard doses of Rituxan, 1 week apart, all your good B-cells are wiped out. They will be gone for about 6 months at which time it starts returning and returns to normal after another 6 months. So we might need to start with that (if I'm not already in the 6 month window) since that will absorb a lot of the Rituxan. On the other hand, this may not be needed at all since the WM cells should be among those killed.
Since I have a long lasting flare (6 weeks after 2 doses the flare starts to decrease) I'm starting with 200mg of Rituxan every 3 weeks and will track my IgM weekly to see how I'm doing. This is 2 small 10mL (100 mg) bottles. There is zero wasted drug.
So this is about 25% of the "standard dose". According to Fig. 1B, I should see a minimum serum Rituxan concentration of about 20mg/mL which should be enough to be effective over the whole 3 week period.
After 2 or 3 doses, I'll get a feel for whether this is reducing your IgM and improving your other counts.
Since Rituxan is safe at lower doses, this appears to be a trial with very little risk. And since we'll know after only a few doses whether it works or not, the risks are even more minimal.
I thought about adding G-CSF to this regimen. The thought is that you give it right after the Rituxan and you give it in a very high dose; the same dose they use for stem cell harvesting. The idea is you shake the WM cells out of the marrow. So this could really enhance the treatment. Guy Sherwood swears by it. However, it could also backfire, e.g., stimulating proteins that might actually help the WM to survive. And if this treatment works, we won't know which thing we did caused it. So Steve Ansell suggests not doing this and just sticking with the 1/2 dose every 3 weeks, but sticking to it for at least 6 months since Rituxan solo is well understood. So I'm going to follow his suggestion.
Can you do this outside of a clinical trial?
It seems harder than heck to get a clinical trial started. And it is very expensive as well. And it tends to be extremely controlled where everyone gets the same dosing schedule and the protocol is defined any results are available so it is not adaptable to individual response and learning that may happen once the trial starts. And nobody seems interested in innovative Rituxan dosing.
Some people tell me "this is irresponsible to do outside of a clinical trial and you'll learn nothing."
I understand their points, but I disagree.
There is nothing magic about a clinical trial. Just because you are in a clinical trial doesn't mean it's any safer for the patient. It does provide a benefit to the doctor in that the clinical trial review board decided it was safe.
However, in my case, I have top WM researchers saying we should try this out and I have one of the most respected MD's in America telling me that if I were their patient, that this would be something that they would try. After all, the standard treatments never cure the disease and the rate of major response is quite low. So I think that provides the scientific justification that this is not an irresponsible thing to do.
Secondly, I disagree that it proves nothing if done outside of a clinical trial. If my IgMs are on the rise at the start of treatment and this treatment reverses the direction of the trend, then that's not just random luck because increasing IgM rarely spontaneously reverses direction downward.
If doing this treatment in one person causes a complete remission without compromising my IgG and IgA levels, then everyone is going to take notice of my experiment of one person done outside of a clinical trial. If that result is successful, it will change the way this disease is treated. So the argument that you gain nothing by doing single patient experiments outside of a clinical trial is completely bogus in my mind. You might gain nothing if you are unsuccessful. But if the treatment is successful, you've done a tremendous service to patients everywhere.
All of this is not to say that clinical trials aren't valuable. They are. People should participate in clinical trials since that is the only way we advance our knowledge of this disease. My point is that it is myopic to view clinical trials as the only way to innovate. If my procedure is successful, hopefully the next step would be a clinical trial to prove it is not a fluke.
Is this medically responsible?
Someone sent me this May 12, 2008 posting from WmCaM group at yahoo. It sums up my EBM treatment at Stanford to a tee. If you want to deviate from the EBM protocols, you have to find a physician who thinks like Dr. Loewy. It's quite possible as I was able to do this without a lot of effort.
Is EBM Compatible with Individualized Patient Care?
Another aspect of the EBM debate that bears close scrutiny is the question of whether it is always in the patient's best interests to be treated according to standardized EBM protocols. On the surface, it seems obvious that patients will benefit when physicians prescribe only those treatments that have been proven through clinical trials to be effective. However, there are those, like Erich Loewy, MD, a bioethicist and professor of medicine at the University of California, Davis, who argue very persuasively that things are not nearly as black and white as they seem, and that EBM, as it is currently practiced, may actually not serve patients well.
In a thought-provoking article for the online medical forum Medscape , Dr. Loewy cites the danger of using EBM as a standard protocol into which any patient with a given disease can simply be plugged. He writes: "To me, as a bioethicist and a physician who has observed the evolution of EBM, I am impressed with the danger to physicians, patients, the educative process, and, ultimately, to the behavior it encourages. Mindless reliance on EBM does exactly what we do not want our students to do: convert what is a suffering human being, with a unique personal life-history, into a specimen of pathophysiology or a heart murmur." (Loewy, 2007).
Dr. Loewy lists a number of ways in which EBM may ultimately result in decisions that are not in the best interests of patients. For example, he writes, "EBM protocols start out being considered as guideposts and end up being considered as straightjackets - and straightjackets that are welcomed by many physicians." One physician actually went so far as to tell Dr. Loewy that he was enthusiastic about EBM guidelines precisely because they saved time and did not require him to think.
Dr. Loewy points out that EBM, as practiced in large institutions, can have the highly undesirable effect of stifling thought and constraining good diagnostic and clinical judgment. Doctors who 'think outside the box' and who feel that a particular patient is uniquely suited for a treatment option that is currently not listed as standard EBM, risk being disciplined by their institution. "EBM is basically anti-intellectual," Loewy writes. Thinking, he reminds us, is among the physician's most important tasks, and EBM protocols, which often consist of nothing more than standard check sheets, actively discourage thinking. Worse, because of the potential for EBM to result in mechanistic treatment decisions that take no account of individual variation, this method "threatens to separate the patient's uniqueness further from the physician and would support looking at the disease instead of at the patient who happens to have that disease."
The essence of CAM is its focus on the individual and its insistence on the rationality and centrality of individualized treatment. Of course it is extremely important to establish treatment guidelines, and to conduct rigorous research into the effectiveness of currently accepted standards of treatment. Teaching physicians to evaluate available treatment options according to whether or not such therapies actually result in measurable benefit to patients might go a long way towards improving care (and reducing costs). But when evidence-based medicine becomes a means of strangling diagnostic skill and reducing patients to algorithms or numbers on a checklist, medicine can no longer call itself the art of healing.
Campath dosing example
Date: Tue, 29 Apr 2008 01:33:44 -0400
From: Rob Selden <[email protected]>
Subject: Re: Standard Protocols -- Whose?
Good questions, Ron.
I've been reading this exchange with great interest, but haven't chimed in till now. Here's yet another thought, of interest to those of us who reacted very badly to Rituxan and can't/won't go near it again. How about a fourth side to the coin?
When Campath (anti-CD52 antibody) was approved, as an IV infusion, it caused Rituxan-like reactions, during and after infusion, in even higher percentages than Rituxan. Eventually (I don't know who, when, or why) the method of administering the drug was questioned. A new method was created, diluting it in far less saline, and administered as a subcutaneous injection. Voila! Reactions were cut to virtually nothing, save for a very small swelling at the injection site which disappeared in minutes as the drug dispersed; a small number of people had minor itching, so the "standard" protocol (though not from the drug manufacturer) is to give Benadryl as a pre-med.
Campath, unlikeRituxan, is humanized. The fully-human versions of Rituxan (e.g., Humax-CD20) seem to cause similar amounts of reactions. Perhaps, after all, it's not the mouse/hamster proteins that some of us are reacting to, but rather the huge instant hit we take via direct infusion into the bloodstream.
So, between 2 of my Campath regimens last year, I questioned my doctor: why not just have the lab use the standard amount of Rituxan itself, but dilute it with just enough saline to give it to me by injection, as with Campath? Needless to say, his first reaction was "it's never been done that way." Words like "bad medicine" also reared their head.
So, it looks like the only way anyone else will ever do something like this is if a clinical trial is done. As far as I can tell, already-approved drugs are held to slightly different standards than new drugs - that is, for use against a different disease, Phase I safety trials don't have to be done, though dose and efficacy (Phases II and III) do need to be tried. However, as I understand it, changes in administration (eg, changing a liquid to a tablet form, or changing IV admin to injection can be filed for approval based on prior approval. (Someone please correct me if I'm wrong here.)
So, I'm not just personally frustrated, but frustrated for all the patients who can't tolerate Rituxan, other Wmers, as well as those with rheumatoid arthritis and other diseases. As Ron asked, who knows what the "standard" Rituxan protocol is? No one, because there isn't one. Rituxan was approved in 1997, almost 11 years ago, but save for the fully human versions being developed and tested by other companies, no one seems to have questioned Genentech about developing true standards for administration nor for modifications that might minimize the adverse reactions to it.
Note: there is also what is basically a humanized version of Rituximab called
Veltuzumab working its way through clinical trials. It is trying to carve out a
niche for itself as friendlier version of Rituxan that can be administered
subcutaneously at lower doses.
Here's the pointer to the phase I/II trial:
http://clinicaltrials.gov/ct2/show/NCT00546793
Message from Ron Draftz
Date: Tue, 29 Apr 2008 13:19:11 -0500
From: Ron Draftz <[email protected]>
Subject: Standard Protocols -- Whose? II
Hi Betty,
Thanks for your comments and yes, I may be the one who started beating the
tom toms for low-dose Rituxan protocols on this TL and if so, I will accept
any criticisms.
The concept of maximum tolerable dose versus low dose is one that suggests
that somehow a cell will become immune to the drug if the drug doesn't
overwhelm the cell. That is a possibility for certain chemo drugs but may
not be applicable for Rituxan.
There are lab tests that show that overdosing tumor cells (the CLL type)
with Rituxan actually pulls the CD20 from the surfaces of those tumor cells,
a process known as shaving. What is left behind is a viable tumor cell that
reproduces but no longer responds to Rituxan. Could that happen with WM
cells. Possibly, perhaps even probably. There is another factor that may
support the use of low-dose Rituxan and that is the way the WM tumor cells
pack or clump in the marrow. That clumping actually blocks the Rituxan from
attaching to enough of the surface of a cell to cause its death. By using a
much lower dose, we can kill just the outer cells of that bunch that are
then lysed and removed exposing the next layer for the next low-dose
treatment. I wouldn't be surprised to discover that the high-dose Rituxan
we now use, leads to cell mutations because the amount of Rituxan on the
cells isn't sufficient to kill the cells. There are reports of CD20
settling into the cell membrane so that Rituxan cannot attach. (I am
deliberately ignoring the vital role played by other cells and signaling
agents, known as the complement effect that are co-contributors to cell
death.)
We really need to know what happens to our tumor and normal cells when
treated with various concentrations of Rituxan especially since the Phase I
trial for Rituxan showed that a dose that was three times less than what we
now use was equally effective in killing tumor cells. However, those tumor
cells were follicular lymphoma cells and we need to know how all this works
for WM cells.
We need to start some of this dose response testing in Petri dishes or test
tubes to see if there is some clue as to whether the cells are more
completely killed with those weekly high doses or perhaps even better with
multiple low-dose treatments three times a week. My reason for suggesting a
test tube approach is that the cost of a clinical trial is absurd and not
something the IWMF can afford. However, the IWMF could support an
exploratory grant done in test tubes and that could perhaps lead to results
that would cause NCI to fund a grant to do a limited patient study.
The stimulus for NCI sponsoring such a grant a is that we might be able to
save billions each year for what Medicare and insurance companies pay for
Rituxan. Of course, our benefit might be that we find the best protocol for
treating WM with Rituxan with the fewest side effects. Until we do these
experiments our doctors are very unlikely to take the risk of trying low
doses for us.
I cannot get my oncologist to use a low dose Rituxan protocol for me in
spite of my offering to have my entire family sign a hold
Rituxan maintenance examples
From Guy Sherwood: There are many different recipes for rituximab maintenance - 1 infusion every 3 month for 2 years (seems to be the most popular recipe) or every 2 months for a year, two years, etc.
From: Bob Reeber: I received 4 infusions of 375mg/M^2 every 6 months for 8.5 years as my maintenance.
Disclaimer
None of this should be construed as medical advice. It is documenting the reasoning I'm using with my doctors. If you think that what I am saying makes sense, you should discuss with your physician whether low-dose Rituxan is right for you.
The medically accepted way to handle new ideas like this is to generate data in animals and then run a clinical trial with sufficiently large number of patients to determine if the approach has merit. Sometimes, just a good argument is good enough, but its easier if you have data. The whole process generally takes about 2 years and assumes they can get enough patients interested. Some people may wish to skip the wait and become a clinical trial of one. It's really your choice. Tom Hoffman has suggested you wait two years and suggesting otherwise is doing you a disservice. That may be true. On the other hand, if taking this advice cures you now, in retrospect, it wasn't a disservice at all and heeding Tom's advice would be disservice. It's your life. You get to choose. Evaluate the data and the arguments.
The biggest risk in taking the approach advocated here is you could become resistant to Rituxan (e.g., you develop HAMA) since low doses over long periods are more likely to develop drug resistance in general. But if that happens, there are other CD20 monoclonal antibodies that should be available soon, e.g., Humax. So I believe the risk is at least mitigated by those options.
Updates
Steve Schneider (the patient from hell) has been getting one std dose (800ml) every 3 months and has a zero CD20 cell count. If he waited 4 months, the CD20 count went positive.
Some people take std dose of Rituxan every 3 months for years and have no problems (such as Steven Schneider who has been taking it for 5 years).
Others have taken a std dose every 2 months and it works.
It would be interesting to take 200mg of Rituxan every 4 weeks (2 small 10mL (100 mg) bottles so no wasted drug) and to measure the actual concentration of the Rituxan in my blood right before each new infusion and see if I achieve 20mg/mL or simply measure the number of CD20 cells. The reason for doing it every 4 weeks is to keep the minimum concentration up to a level that keeps killing throughout the period. Although this is slightly less total drug than Schneider gets over the same period, there is probably more effectiveness since the drug is eliminated proportional to the concentration so given a fixed amount of drug, it is more efficient to dispense it evenly over time. There would be less chance of shaving since the peak concentration is lower. And there should be less side effects since the peak concentration is lower. The 200mg also will reduce flare, an important consideration in my case.
By measuring my CD20 concentration before each infusion, I can determine whether to increase or decrease the time between infusions or increase the dosage.
Links
Waldenstrom's macroglobulinemia: Steve Kirsch's story
Waldenstrom's macroglobulinemia: My treatment plan